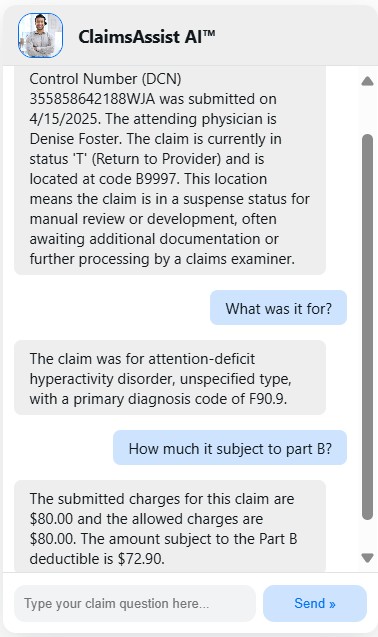
Helping Medicare Providers understand their claims is more important than ever. ClaimsAssist AI™ gives your Providers and your customer service staff the clarity they need — through user-friendly, secure, and compliant conversations.
ClaimsAssist AI™ interfaces with your claims systems, augments responses with easy-to-understand jargon, and delivers real-time, personalized answers across channels like voice, chat, or mobile — without hold times or confusion.
Why ClaimsAssist AI™ For Medicare?
Medicare Providers often have complex questions. From understanding deductibles to getting clarity on claim denials or coverage explanations, every interaction must be:
- Clear
- Personalized
- Compliant
- Accessible
ClaimsAssist AI™ empowers you to meet CMS expectations while enhancing member experience and reducing call center strain.
Let ClaimsAssist AI™ Support Your Medicare Mission
Reduce operational strain, support your call center teams, and most importantly — help your Medicare providers get the answers they need without stress or delay.
Interprets claim detail information and presents it to users in a clearly understandable language. We accomplish this through back-end data aggregation to pull real-time data from multiple systems (claims adjudication, member records, appeals).
ClaimsAssist AI™ is built with CMS, OCR, and HIPAA guidelines in mind. Our stress-free integration complies with all regulatory guidelines while offering natural language support.
Click the link below to download our one-page information sheet about Claims Assist AI.
Providers can ask any question in their own words, and get a precise, conversational answer. Conversational tone, large text compatibility, and clear language makes ClaimsAssist AI™ friendly for all age groups.
ClaimsAssist AI™ is accessible via Voice (IVR), Web Chat, and Mobile App. Staff or contact center agents will be notified if attention is needed beyond the AI assistant.
